KAIST
BREAKTHROUGHS
Research Webzine of the KAIST College of Engineering since 2014
Spring 2025 Vol. 24Porous silicon-based nanomedicine reversing rheumatoid arthritis
Porous silicon nanoparticle coated with calcium silicate shell was proposed for severe rheumatoid arthritis (RA) as a drug delivery platform. The use of calcium silicate-coated nanoparticle improved RA drug efficacy utilizing inflamed tissue-specific environment (neo-vasculature and low pH). More importantly, it was the first time observation that porous silicon nanocarriers themselves can modulate immune cells and reverse bone loss.
Therefore, unlike conventional RA medicine, the developed porous silicon-based nanomedicine could co-modulate the RA progression and bone erosion, which was effective on RA amelioration.
Article | Spring 2023
Rheumatoid arthritis (RA) is one of the inflammatory autoimmune diseases that cause patients discomfort due to the severe bone erosion. Although the incidence of RA is increasing every year, the therapeutics providing a complete remission still remain elusive. RA drugs used in clinics might ameliorate the disease’s progression, but they still have limitations such as low drug efficacy in RA joints and negligible effect on damaged bone tissue. For these reasons, a new medicine should be developed that can co-modulate the RA progression and damaged joint tissue. A research team, led by Professor Ji-Ho Park at KAIST, recently proposed porous silicon-based nanomedicine for the first time, which can simultaneously manage RA progression and bone erosion. This report highlighted the impact of porous silicon-based nanomedicine as bone turnover therapeutics as well as RA drug carrier. This study entitled “Porous silicon-based nanomedicine for simultaneous management of joint inflammation and bone erosion in rheumatoid arthritis” was published in ACS Nano on October 10, 2022 https://doi.org/10.1021/acsnano.2c04491.
The research group utilized porous silicon nanoparticle as a drug (methotrexate, MTX; gold standard RA drug) carrier for the treatment of RA as shown in Figure 1. First, they focused on the RA joint-specific drug delivery by utilizing the leaky vasculature and low pH of inflammatory tissue (RA joint). Then, they trapped MTX drug in the porous structure of the porous silicon nanoparticle during the formation of calcium silicate shell on the nanoparticle (pCaSiNP-MTX). Therefore, drug accumulation in RA joint was increased as nanoparticles accumulated more compared to the free drug. In addition, the low pH-sensitive calcium silicate dissolution increased the release of MTX in in the RA joint. The RA joint-specific drug delivery increased drug efficacy, and showed effective disease amelioration in a severe RA model.
More importantly, the researchers observed the therapeutic effect of pCaSiNP for itself against RA progression and bone remodeling for the first time as shown in Figure 2. They found that pCaSiNP reduced effector T cells, which are one of the major pro-inflammatory cells promoting RA progression. Additionally, pCaSiNP inhibited the differentiation of osteoclast (bone-resorption cell) but promoted calcium mineralization of osteoblast (bone-formation cell), which reversed the broken balance between bone resorption and formation in RA. pCaSiNP-MTX treatment with a low dose of MTX showed effective amelioration of RA compared to pre-existing studies due to the simultaneous modulations of MTX and pCaSiNP against RA disease and bone erosion. This pCaSiNP-based nanomedicine may also be effective carriers for other antiarthritic agents, which underscores the translational potential of this porous silicon-based nanomedicine for RA treatment.
Dr. Moonkyoung Jeong from the Department of Bio and Brain Engineering participated in this study as the first author. This study was supported by the Basic Science Research Program through the National Research Foundation funded by the Ministry of Science and ICT (NRF-2017R1E1A1A01074847, NRF-2018R1A6A1A03025124, and NRF-2021R1A2C2094074). This study was partially supported by the NSF through the UC San Diego Materials Research Science and Engineering Center (UCSD MRSEC, DMR-2011924).
*Figures were revised from the original manuscript. Copyright: 2022 American Chemical Society
Most Popular

When and why do graph neural networks become powerful?
Read more
Smart Warnings: LLM-enabled personalized driver assistance
Read more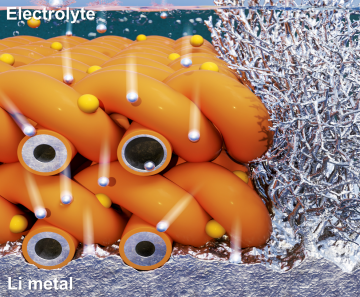
Extending the lifespan of next-generation lithium metal batteries with water
Read more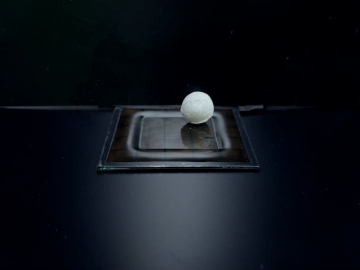
Professor Ki-Uk Kyung’s research team develops soft shape-morphing actuator capable of rapid 3D transformations
Read more
Oxynizer: Non-electric oxygen generator for developing countries
Read more
![[Figure 1.] Development of pCaSiNP-MTX and improvement of MTX efficacy by increased accumulation and pH-sensitive drug release](http://breakthroughs.kaist.ac.kr/wp/wp-content/uploads/2023/03/%EA%B7%B8%EB%A6%BC32.png)
![[Figure 2.] Co-modulation of RA progression and bone erosion of pCaSiNP-MTX in mouse RA model.](http://breakthroughs.kaist.ac.kr/wp/wp-content/uploads/2023/03/%EA%B7%B8%EB%A6%BC4.png)